Contact Us
- Home
- Contact us
Best Heart Transplant surgeon in South Mumbai
A best doctor for heart transplant involves surgery to remove a patient's damaged heart and replace it with a healthy donor heart. The donor must be deemed brain dead by two or more medical professionals before the donor's heart can be removed.
A medical professional must determine that a heart transplant is the best course of action for treating your heart failure before they can put you on the waiting list. Additionally, a medical team verifies that you are in good enough overall health to undergo the transplant procedure.
Why Would I Require A Heart Transplant?
If other treatments are failing and your heart is failing, you might need a heart transplant. Heart failure can have a few causes, such as:
(Myocardial Infarction, or MI) Heart attack
Infection of the cardiac muscle by a virus
Elevated blood pressure
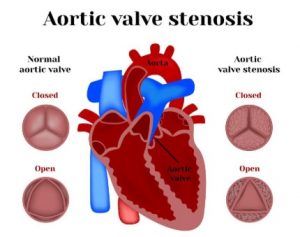
Heart valve dysfunction
Birth abnormalities in the heart (congenital)
Heart irregularities, or arrhythmias
Elevated pulmonary blood pressure, or pulmonary hypertension
Substance misuse or alcoholism
Emphysema and chronic obstructive pulmonary disease are examples of chronic lung illnesses (COPD)
Thicker, more rigid, and enlarged heart muscle (cardiomyopathy)
Anemia, or low red blood cell count
There can be further justifications for best doctor to suggest a heart transplant.
What Dangers Come With Having A Heart Transplant?
Like with any procedure, there could be after effects. The following are possible hazards of a heart transplant:
Virus Infection
Bleeding either during or during surgery
Blood clots that may result in lung issues, heart attacks, or strokes
Breathing issues
Renal failure
CAV stands for coronary allograft vasculopathy. The blood arteries that supply the cardiac muscle with blood are the source of this issue. They solidify and thicken. This may seriously harm the heart's muscles.
Failure or rejection of the donor heart
Demise
Why Do Heart Transplants Take Place?
When other heart-related therapies are ineffective and cause heart failure, a heart transplant is carried out. Heart failure may be brought on by the following factors:
Heart muscles that are weak
Heart Valve Disease
Heart Valve Disorder
Birth Disorders of the Heart
Uncontrollably occurring cardiac rhythms.
An earlier heart transplant attempt that failed
When the patient's own sick heart is unable to sustain adequate bodily functions, heart transplant surgery is carried out.
How should I prepare for heart surgery?
A heart transplant is not appropriate for every person. To decide whether a person is eligible for a transplant, many different pieces of information are required. An organ transplant team will assess the data. The team consists of a social worker, a psychiatrist or psychologist, a transplant surgeon, a transplant cardiologist (a physician who specializes in treating cardiac conditions), nurse practitioners or physician assistants, one or more transplant nurses, and a physician assistant. Dietitians, chaplains, hospital administrators, and anesthesiologists—physicians who employ drugs to put patients to sleep during surgery—may also be on the team.
The procedure for evaluating transplants will comprise:
Social and psychological assessment. Stress, money problems, and support from family or close friends are a few psychological and social challenges associated with organ transplantation. These elements may have a significant impact on your post-transplant outcome.
Blood examinations to locate a suitable match and increase the likelihood that the donor heart won't be rejected, blood testing will be required.
Examinations for diagnosis. Tests will be necessary to evaluate your general health and lung health. X-rays, ultrasounds, CT scans, pulmonary function tests (PFTs), right cardiac catheterization, and dental examinations are a few examples of these tests. Women might require a mammography, gynecological assessment, and Pap test.
Additional arrangements. Multiple vaccinations will be administered to lower the risk of infections that could harm your newly transplanted heart.
If the transplant team determines that you are suitable for a heart transplant, they will take into account all the data gathered from your medical history, physical exam findings, and results of your diagnostic tests
Signs And Symptoms
In order to be promptly sent to the transplant list, it is critical to comprehend the indications for heart transplantation. A prompt referral ensures that the patient can live on mechanical support or inotropes until the heart is available. Prior to submitting a patient, it is important to confirm that they do not have any conditions that might prevent them from receiving a heart transplant.
Chronic Heart Failure
Patients who fall into the following group with chronic heart failure should be referred for a heart transplant in outpatient settings:
Individuals receiving guideline-directed medical therapy (GDMT) but still experiencing exertion-limiting symptoms. (Patients in stage D of the American College of Cardiology or in classes 3 or 4 of the New York Heart Association).
Individuals who adhere to GDMT but have repeated readmissions for heart failure exacerbations (two or more in a 12-month period)
Cardiorenal syndrome-related decline in renal function.
The use of GDMT is prohibited by dose-limiting adverse effects such as hypotension and contraindications such as renal failure.
Progressive deterioration of right ventricular function (cor pulmonale) or left heart failure-related rise in pulmonary artery pressure.
Ventricular arrhythmias that recur often even with the best medication and electrophysiological care.
Acute Heart Failure
Patients who need an immediate referral for a heart transplant in an inpatient setting include:
Refractory cardiogenic shock in spite of inotropic therapy at maximum dose.
Refractory cardiogenic shock with mechanical circulatory assistance applied topically.
Refractory pulmonary edema, which needs ventilation and positive pulmonary pressure, does not respond to diuretics.
Refractory ventricular arrhythmia that is unresponsive to electrophysiological or medicinal treatments.
Therapy
The general procedural technique for the two types of implantation operations is as follows:
Orthotopic Heart Transplantation: This is a far more widely used process. All of the recipient's heart is removed, with the exception of the left and right atria's cuffs. Anastomosing the donor and recipient's right atrium to the recipient's left atrial cuff, aorta, and pulmonary artery (PA) allows for the transplantation of the donor's heart. The recipient's right atrium is completely removed after this, and the recipient's vena cava is anastomosed to the donor's right atrium using a bicaval procedure.
Heterotopic Heart Replacement Surgery: There have only been a few operations carried out globally, making this an uncommon surgery. The donor heart is implanted into the patient's thoracic cavity, without the recipient's heart being removed. The donor and recipient atria undergo anastomosis. Both the donor PA and the recipient PA are anastomosed to the recipient aorta and PA, respectively.
Below is a thorough explanation of the orthotopic heart transplant.
Heart Excision in the Recipient
Using a sternotomy and pericardiotomy, the chest is opened to begin the excision process. The superior and inferior vena cavae are mobilized and taped shut, and the aorta and pulmonary veins are divided. At the proper active coagulation time (ACT), heparinization is started, and the aortic cannula is introduced into the aorta. Right-angled cannulas that are placed close to tape snare and far above the cavo-atrial junction are used to cannulate the superior vena cava (SVC). The inferior vena cava (IVC) is cannulated above the diaphragm reflection using a straight purse-string cannula.
Cardiopulmonary bypass is initiated with the donor heart 10 to 15 minutes after it arrives, at 32 degrees Celsius (hypothermia). The left heart is decompressed when the left atrium is removed at the intersection of the right superior pulmonary vein. Both directions are included in this incision. The cavo-atrial junction separates the SVC. The right atrial cuff is left in place after the right atrium is removed above the IVC tape snare. Just above the valves, the aorta and pulmonary artery are removed. The distal vessel still has a good amount of length left. Ultimately, the left atrium is excised by extending its incision lower and medially into the appendage. This joins the four pulmonary veins to form a sizable cuff, and the heart is removed.
The Heart of the Donor
After connecting the pulmonary veins, the donor heart is excised, and the left atrial cuff is trimmed to match the recipient's. The foramen ovale and mitral valve are examined to ascertain whether they are closed or patent. The aorta and pulmonary artery are among the large vessels that are removed.
Recovery And Finalization
The heart is reperfused because the large vessels are unclamped. While the rewarming procedure is ongoing, the heart is reperfused for a minimum of half an hour. The ventricles are decompressed by de-airing as well. The bypass is gradually removed from the patient. After the bypass is turned off, two mediastinal drains are implanted, and protamine is given to counteract the heparin. The chest is secured in the conventional manner.
To reduce the risk of surgical wound infections, close observation, post-operative care, and guidance are necessary. For suture and drain removal, a follow-up appointment with a cardiothoracic surgeon is usually necessary in four to six weeks.
Why Select Your Heart Surgeon from Dr. Amit Karad Shad?
Once Dr. Amit Karad has a thorough understanding of his patient's condition and medical history, he performs heart transplant surgery. We typically need several days to evaluate a patient with heart failure. In order to try and identify potentially treatable causes for heart failure, we also perform a full biochemical screening. We check medical records, treatments received, and other medical/surgical conditions that might prohibit transplantation (such as advanced age, cancer, active infections, serious kidney or liver failure, alcohol abuser unwilling to stop alcohol). When it becomes evident that a patient can only benefit from a heart transplant, the patient is added to the active transplant waiting list in order to receive a donor organ claims South Mumbai-based physician Dr. Amit Karad, who specializes in heart transplants.

